ICU - Non-Invasive Ventilation (NIV) Secrets:
Did you ever admit to the ICU a patient with COPD exacerbation who came from the ED on NIV? Or who went home on NIV? If you are a pulmonologist, you will not learn anything from this post but the rest of us x.com
Did you ever admit to the ICU a patient with COPD exacerbation who came from the ED on NIV? Or who went home on NIV? If you are a pulmonologist, you will not learn anything from this post but the rest of us x.com
from different specialties (I am Internal Medicine) should remember that NIV settings are not just inspiratory/expiratory pressure (IPAP/EPAP) and FiO2
We have to admit that not every COPD patient will do well with “10 over 5” *. So what else should we pay attention to? x.com
We have to admit that not every COPD patient will do well with “10 over 5” *. So what else should we pay attention to? x.com
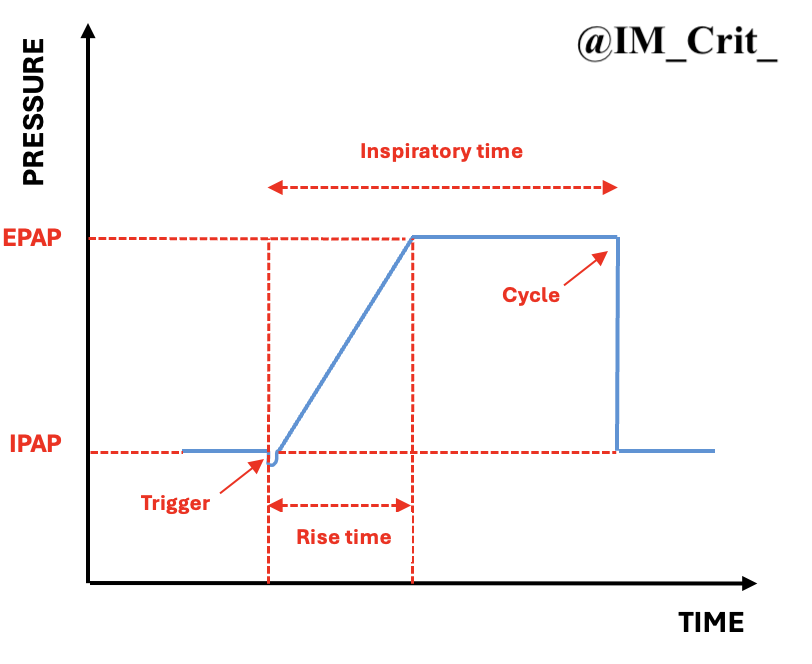
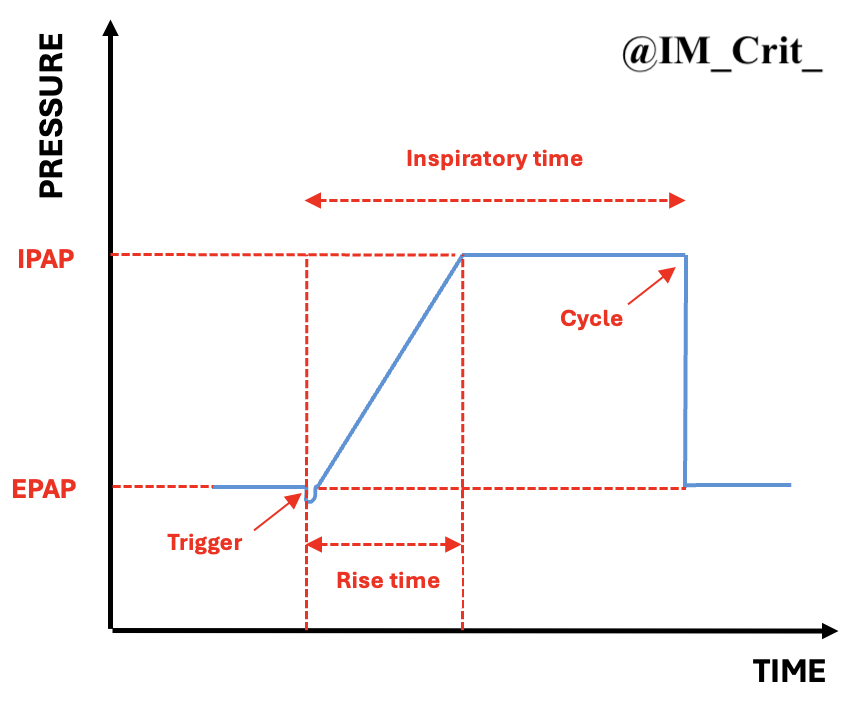
Trigger: beginning of inspiratory support and switch from EPAP to IPAP
Rise time: the time to get from EPAP to IPAP (aka pressurization time)
Inspiratory time: duration of inspiratory support
Cycle: end of inspiratory support and return from IPAP to EPAP x.com
Rise time: the time to get from EPAP to IPAP (aka pressurization time)
Inspiratory time: duration of inspiratory support
Cycle: end of inspiratory support and return from IPAP to EPAP x.com
IPAP:
Of course, achieving significant PCO2 reduction is a main goal of NIV, along with resting the respiratory muscles. This usually requires high driving pressures; that means that even if we start with an IPAP of 10, we should not be scared to go for an IPAP of ~20-25 cmH2O
Of course, achieving significant PCO2 reduction is a main goal of NIV, along with resting the respiratory muscles. This usually requires high driving pressures; that means that even if we start with an IPAP of 10, we should not be scared to go for an IPAP of ~20-25 cmH2O
(very rarely >30) to overcome high airways resistance. This will hopefully result in larger tidal volumes >8 ml/kg
EPAP (or: PEEP):
EPAP traditionally is set at low values (~ 5 cmH2O) in COPD patients. However, higher EPAP may be needed if the patient is obese and/or there is need to correct upper airway obstruction
EPAP can also help to:
EPAP traditionally is set at low values (~ 5 cmH2O) in COPD patients. However, higher EPAP may be needed if the patient is obese and/or there is need to correct upper airway obstruction
EPAP can also help to:
i) "match" intrinsic PEEP, reducing triggering effort & asynchrony, &
ii) counteract expiratory flow limitation by stenting open the airways and decreasing hyperinflation
Finally, a minimum EPAP of 3-4 cm H2O is usually necessary to prevent rebreathing in a single-limb circuit
ii) counteract expiratory flow limitation by stenting open the airways and decreasing hyperinflation
Finally, a minimum EPAP of 3-4 cm H2O is usually necessary to prevent rebreathing in a single-limb circuit
Back-Up Rate:
This seems to be less important (in achieving adequate minute ventilation) than the IPAP &, if set too high, it can lead to intolerance. Most patients come on S/T mode (spontaneously triggered with a timed backup respiratory rate); a rate of ~12 is reasonable
This seems to be less important (in achieving adequate minute ventilation) than the IPAP &, if set too high, it can lead to intolerance. Most patients come on S/T mode (spontaneously triggered with a timed backup respiratory rate); a rate of ~12 is reasonable
Rise Time:
A rapid pressure rise from EPAP to IPAP provides high flow when inspiration is triggered, reducing the work of breathing & by reaching faster the target IPAP this potentially it may lead to a higher delivered volume
A rapid pressure rise from EPAP to IPAP provides high flow when inspiration is triggered, reducing the work of breathing & by reaching faster the target IPAP this potentially it may lead to a higher delivered volume
A time of 0.2 sec is commonly used (some ventilators use unitless numbers or percentages, so check out with the ventilator manual or the respiratory therapist to see what they actually mean)
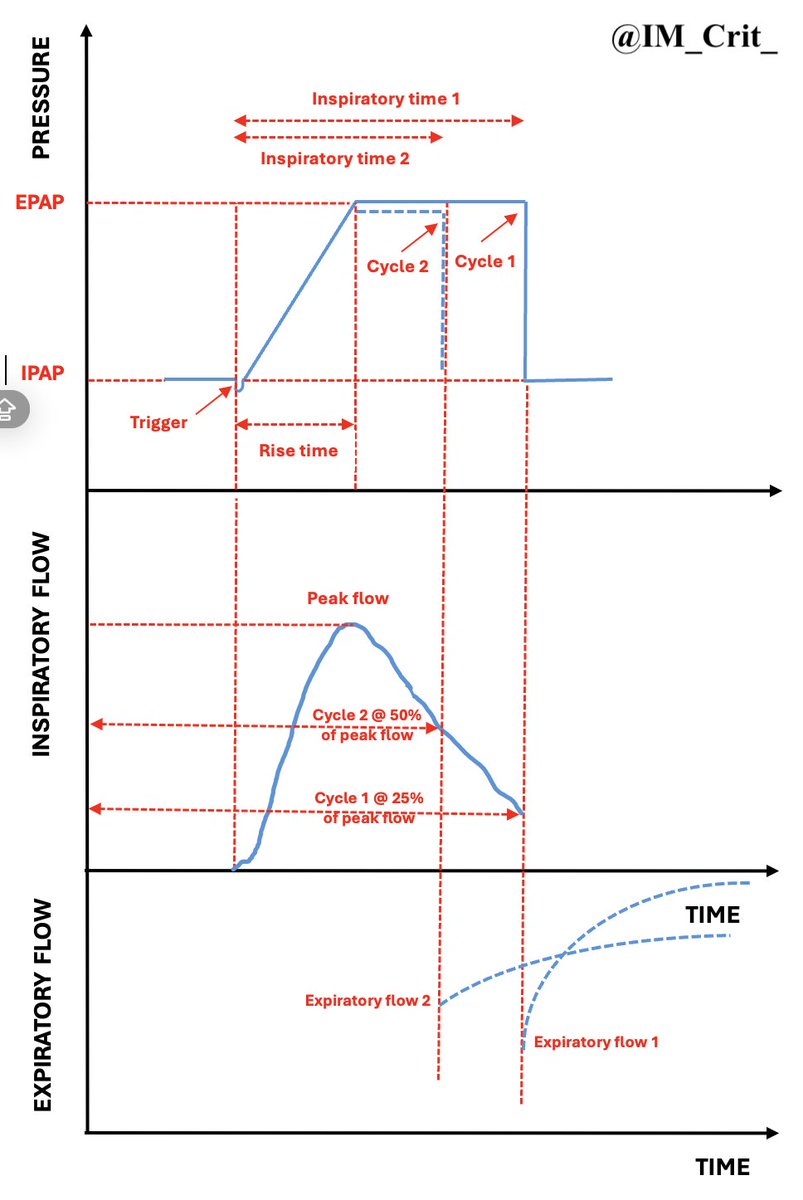
Inspiratory time – Cycle-off:
COPD patients need longer expiratory times to exhale; in other words, the Ti should be shortened, provided that ventilation remains adequate. Delaying the return from the inspiratory to the expiratory phase
COPD patients need longer expiratory times to exhale; in other words, the Ti should be shortened, provided that ventilation remains adequate. Delaying the return from the inspiratory to the expiratory phase
(cycling off from IPAP to EPAP) can lead to asynchrony. Cycling off the insp flow, therefore, should be set at higher sensitivity (earlier) & the peak flow is used as the "reference" signal. Please see in my poor graph how moving from cycling off #1 to #2 ⬇️ inspiratory time x.com
* "10 over 5" usually means EPAP of 5 cmH2O plus another 5 cmH2O of pressure support leading to a total IPAP of 10 cmH2O. However, in some vent settings, this may mean 10 "on top of" 5 for a total IPAP of 15 cmH2O, so it's always good to check what the actual numbers are...
I obviously flipped the position of the IPAP - EPAP in the graph. Sorry…
Loading suggestions...