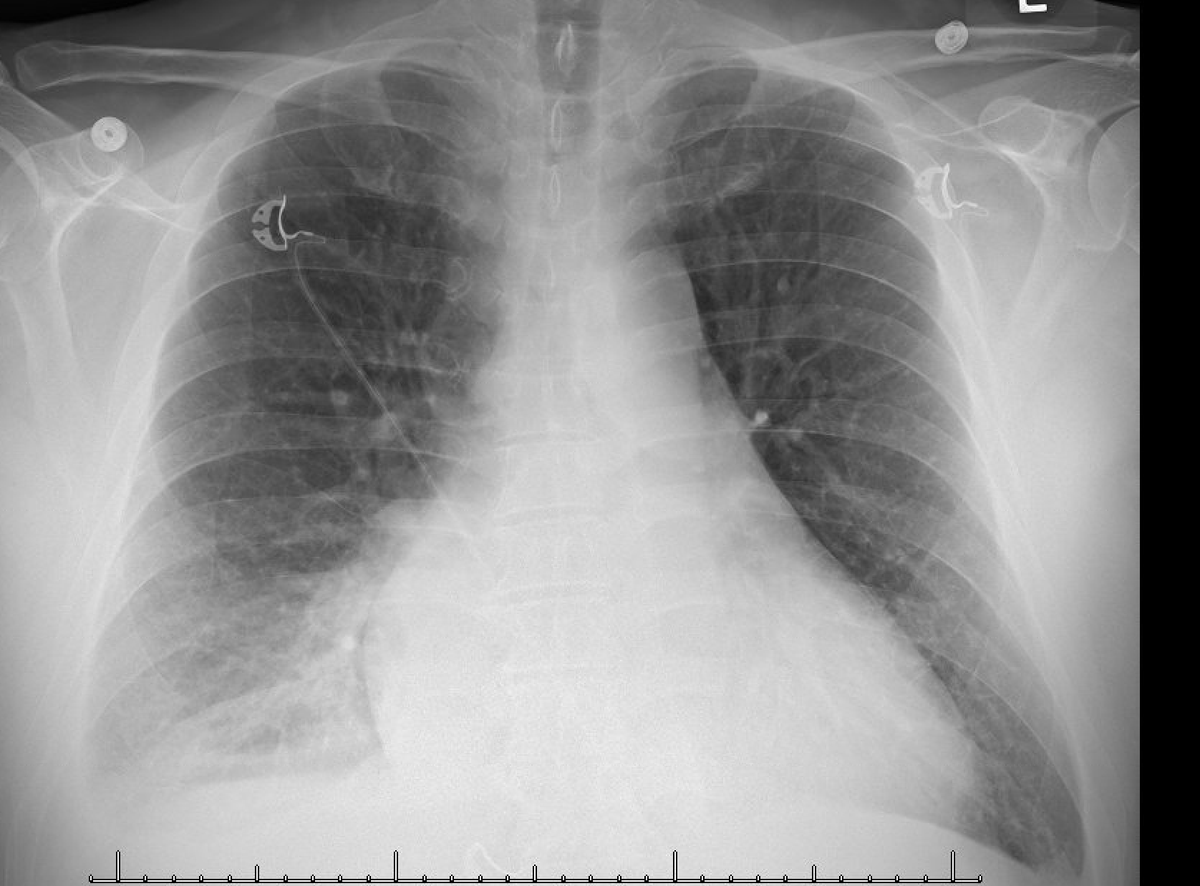
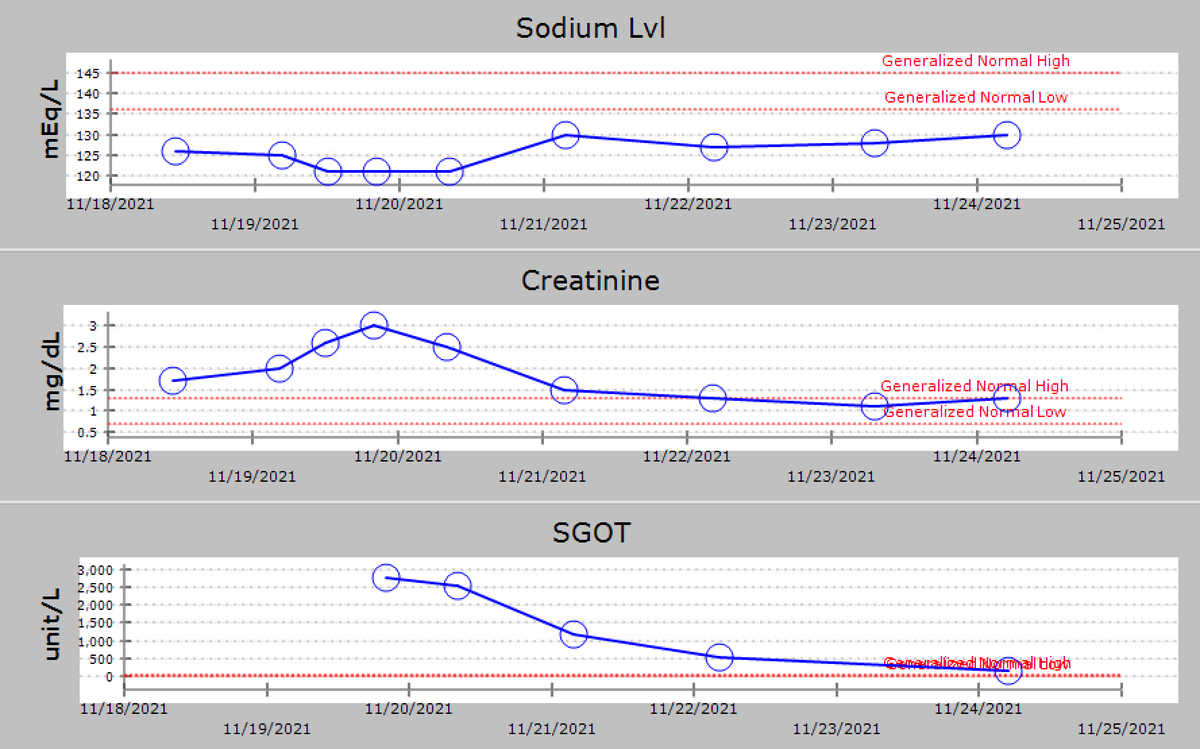
trop 60 (nl<20), BUN/creat 28/1.7 (baseline 10/1.0). Received ivf bolus for sepsis/PNA, antibiotics and diltiazem drip (Cards order). Placed in isolation. Next am Cards stopped ivf & gave Lasix 20 mg iv. UOP was reported poor. Creat ⬆️, Na ⬇️ further, AST/ALT checked & found ⬆️⬆️
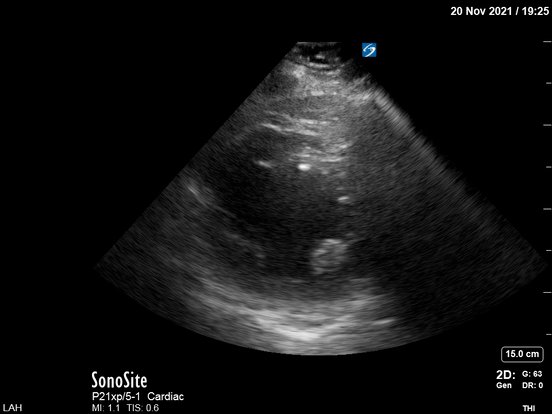
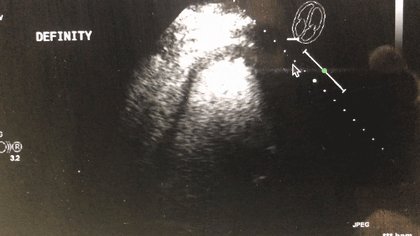
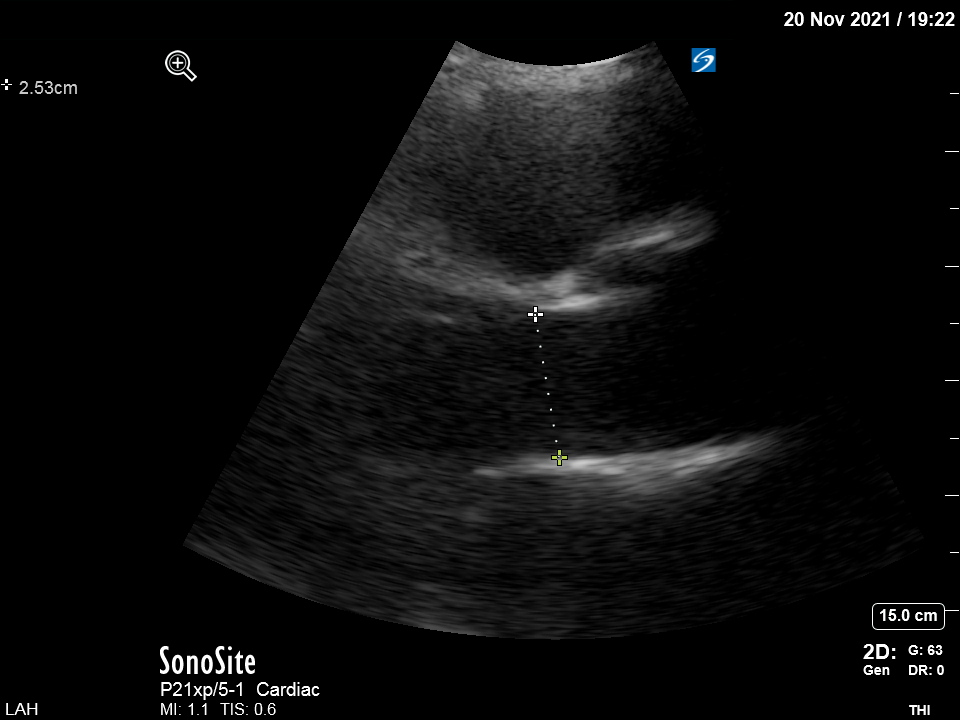
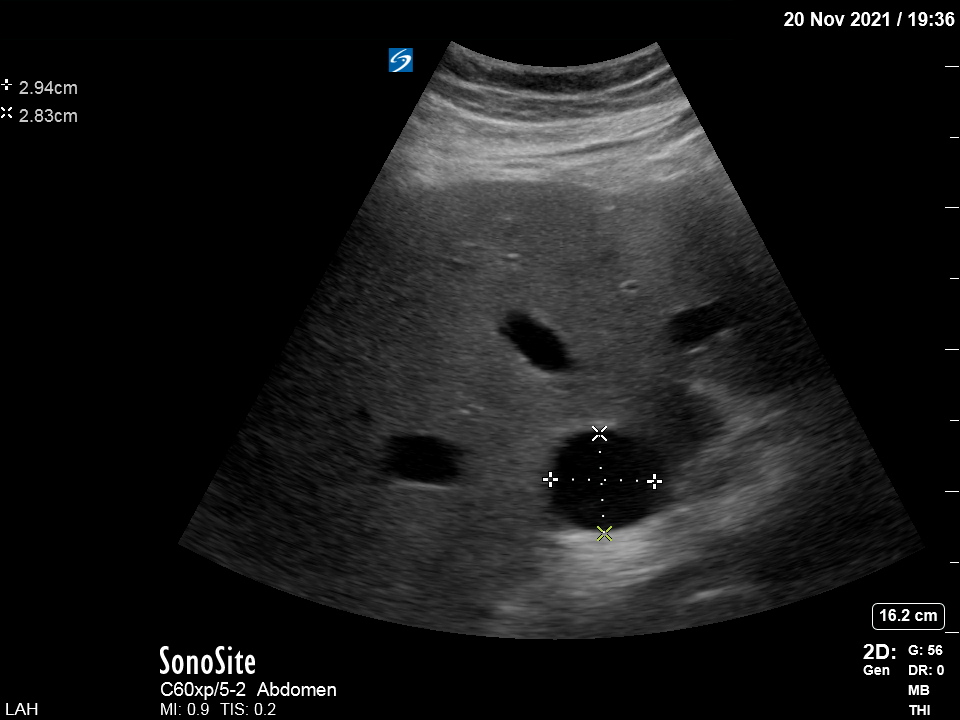
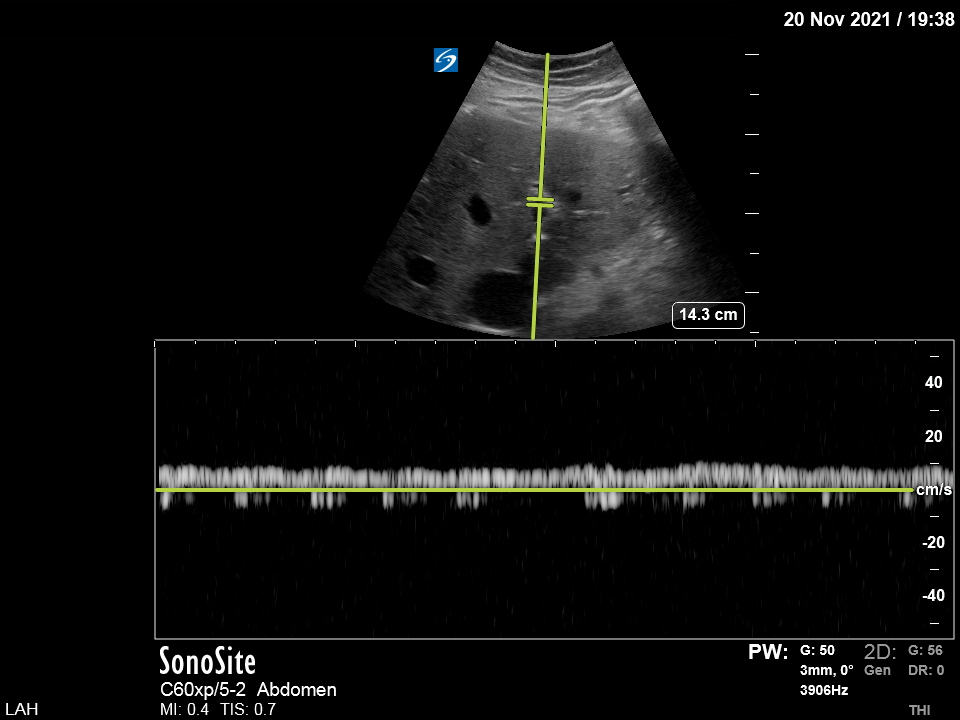
Pt was transferred out of the ICU and a couple of ds later, a cardiac cath showed CO/CI 4.4/1.9. The etiology of CHF is still unclear. GI follow the pt for a newly diagnosed "cirrhosis" probably explaining why portal vein was not pulsatile!
Take-home message:
In cases of poor LV systolic function w organ hypoperfusion, there is usually an urge to use inotropes/vasodilators to increase “forward flow”. In some of these cases a trial of high doses of iv diuretic can make the trick without need for advanced hemodynamic
In cases of poor LV systolic function w organ hypoperfusion, there is usually an urge to use inotropes/vasodilators to increase “forward flow”. In some of these cases a trial of high doses of iv diuretic can make the trick without need for advanced hemodynamic
monitoring (besides POCUS +/- A line). Sometimes in pts w renal dysfunction, neurohormonal maladaptive mechanisms come into play & lead to increased Na reabsorption, decreased H2O clearance, and diuretic resistance (all three probably shown in this case). If/when diuretics start
to work, you may see impressive diuresis (nurses say that pt "opened up"…). I guess a combination of some decongestion in the venous side and improvement of forward flow by blunting of sympathetic activation may increase renal perfusion and diuresis
As always, this was just one way to manage this patient and there may be better ways than mine!
Thanks for reading!
Thanks for reading!
I decided to write this case tonight after reading a thread from @NephroP @ArgaizR @ThinkingCC @critconcepts @Rajiv_sinavan. Thank you!
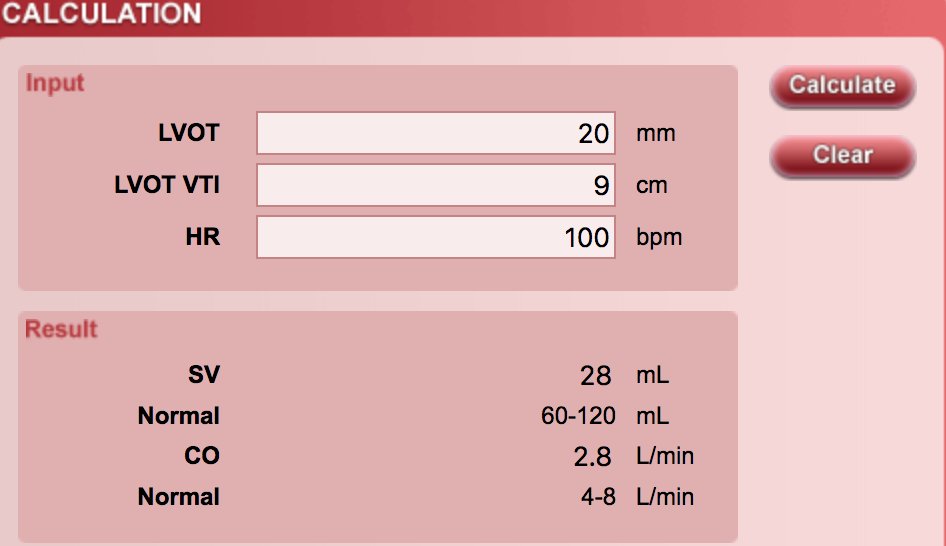
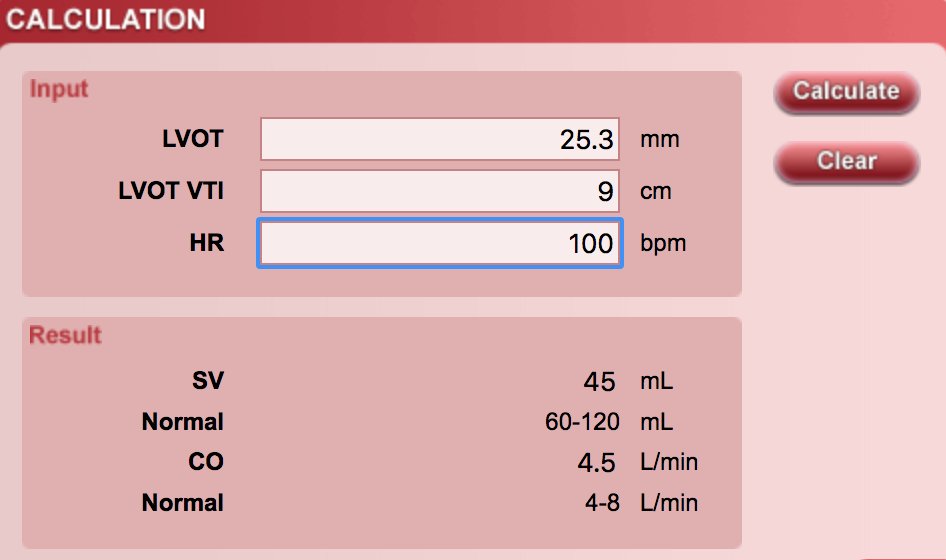
I used the csecho.ca for the CO calcs. Thank you!
I used the csecho.ca for the CO calcs. Thank you!
Loading suggestions...