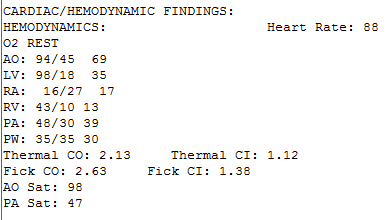
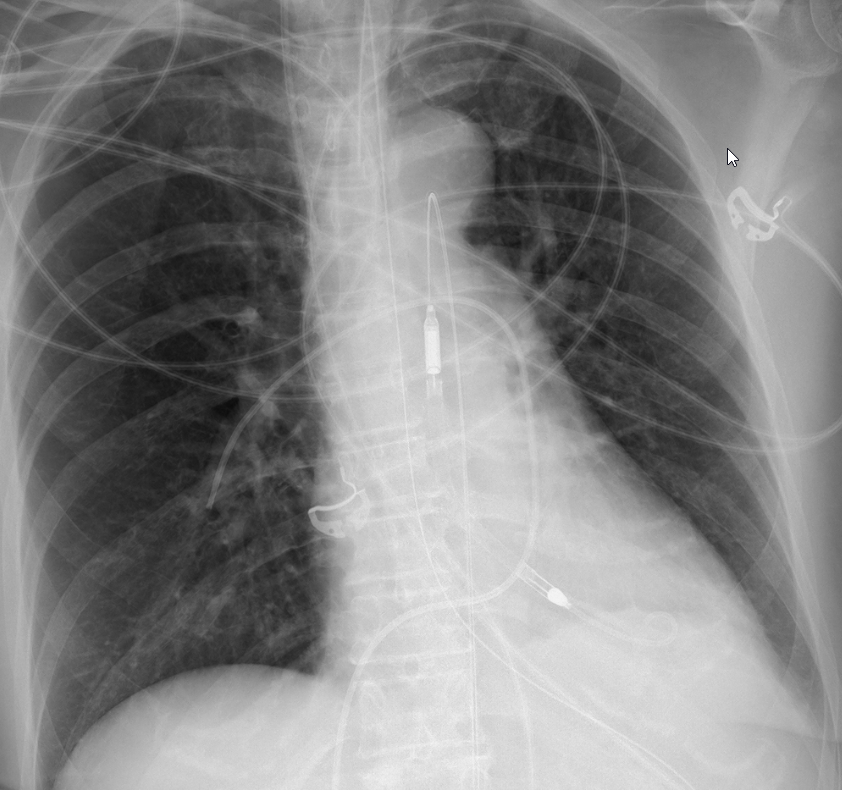
ICU stories: Middle-aged pt w remote hx of seizures had grand-mal sz at home & in the ambulance. Intubated for airway protection in ED; transferred to ICU. Placed on propofol. Overnight received 5 l NS & norepi gtt @ 0.1 & (ABx + steroids) for septic shock due to aspiration PNA.
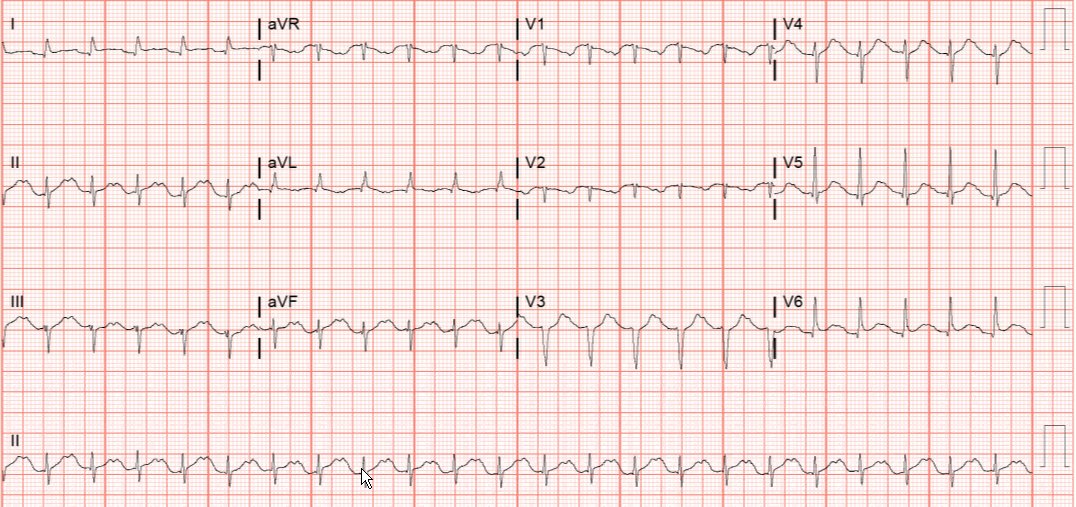
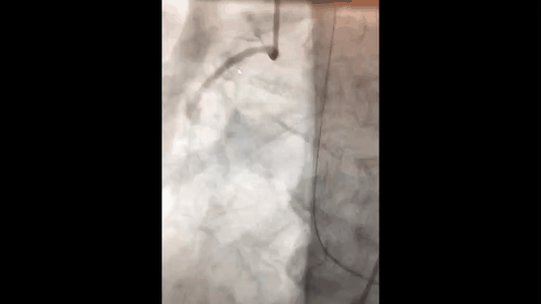
POCUS: severe LV dysfunction (LVEF < 20%). An episode of atrial fib led to worse hemodynamics; amio and heparin drips started and rhythm converted to SR. Pt transferred to OH for cath. Can you guess where the culprit lesion was?
The Impella was removed 2 ds later. Patient was extubated and gradually improved
Take-home message:
1. Stress-cardiomyopathy is a fairly common cause of unexplained hemodynamic instability
2. It is extremely unlikely for a patient to develop septic shock from aspiration PNA just a few hours after a seizure episode
Thanks for reading!
1. Stress-cardiomyopathy is a fairly common cause of unexplained hemodynamic instability
2. It is extremely unlikely for a patient to develop septic shock from aspiration PNA just a few hours after a seizure episode
Thanks for reading!
Loading suggestions...